Federal Medicaid Outlays During the COVID-19 Pandemic
This data note analyzes federal Medicaid spending in fiscal 2020 (FFY) before and during the COVID-19 pandemic. Overall, federal Medicaid spending was $ 458 billion, up 12.0% in FY 2020, up from 5.2% in FY 2019. That increase in annual spending was largely due to accelerated growth in the second half of the fiscal year attributed to the start of the pandemic and the start of increased federal Medicaid funding in late March. Monthly growth in federal Medicaid spending also increased over this period, reversing previous trends of a slowdown in monthly growth.
The expense data analyzed in this data note comes from the US Government's monthly statement of income and expenses. The Bureau of the Fiscal Service (part of the US Treasury Department) publishes these monthly financial reports that summarize the financial activities of the US federal government, including the income and expenditure of funds. In particular, this data note analyzes Treasury data on federal government spending classified as "State Grants for Medicaid". This analysis examines the annual growth as well as quarterly growth for Fiscal Year 2020 versus Fiscal Year 2019 to understand the impact of the pandemic and the federal expanded matching funds. Although the changes to the federal Medicaid guidelines in FFY 2019 resulted in incremental changes in registration and spending, there weren't any major policy changes that year, making it a useful foundation. Examining the quarterly growth for the biennium allows a comparison between the 2020 FFY and a possibly more typical quarterly variation.
As part of the federal response to the COVID-19 pandemic, states will have access to expanded federal funding from Medicaid. States and the federal government jointly fund Medicaid. The pandemic has sparked both a public health crisis and an economic crisis that has had a significant impact on Medicaid, a countercyclical program. During the economic downturn, more people enroll in Medicaid as incomes fall, which can increase program spending while reducing government tax revenues. To support Medicaid and ensure broad tax relief as government revenues fell sharply, the Families First Coronavirus Response Act (FFCRA) approved an increase in the Medicaid Available Match Rate ("FMAP") by 6.2 percentage points (retroactive to Jan. January 2020) if states meet certain requirements for maintaining eligibility (MOE). This FMAP increase doesn't apply to the Affordable Care Act expansion group, for which the federal government already bears 90% of the cost. The states could use the increased federal settlement funds from the end of March for claims paid in the first quarter of 2020 and in early April for the second quarter of 2020.
Federal Medicaid spending grew 12.0% annually in FFY 2020 compared to 5.2% in FFY 2019, with growth rates significantly higher in the second half of the year (Figure 1). Total spending in the first quarter (October to December 2019) increased 5.2% year over year and total spending in the second quarter (January to March 2020) increased 4.5%. First quarter growth was higher than last year (FFY 2019), but second quarter growth was similar to last year.
However, following the outbreak of the COVID-19 pandemic and the passage of the FFCRA in March 2020, federal Medicaid spending rose faster in the second half of FFY 2020. Total spending in the third quarter (April to June 2020) increased 22.5% year over year (with a 8.7% growth in the third quarter). This significant increase likely reflects the Medicaid retrospective claims that were made available in late March and that were improved for the second quarter. The higher year-on-year growth continued in the last quarter (14.9% in FFY 2020 compared to 6.7% in the previous year), which is due to the continuously improved federal match as well as the increased enrollment due to the requirements that the states Medicaid continuously cover participants to gain access to the improved game and also to the economic downturn. National data shows a 6.1% increase in Medicaid registrations from February to July 2020, a reversal of pre-pandemic trends when registrations declined.
Figure 1: Federal Medicaid spending growth increased in the second half of FFY 2020 compared to FFY 2019
Higher average monthly growth at the end of FFY 2020 reverses the trend of a slowdown in average monthly growth in the previous three quarters (Figure 2). Month-to-month average growth slowed from the start of 2019 to the first half of 2020 when average monthly growth was negative. The pandemic and the increased match rate reversed this trend in average monthly growth rates.
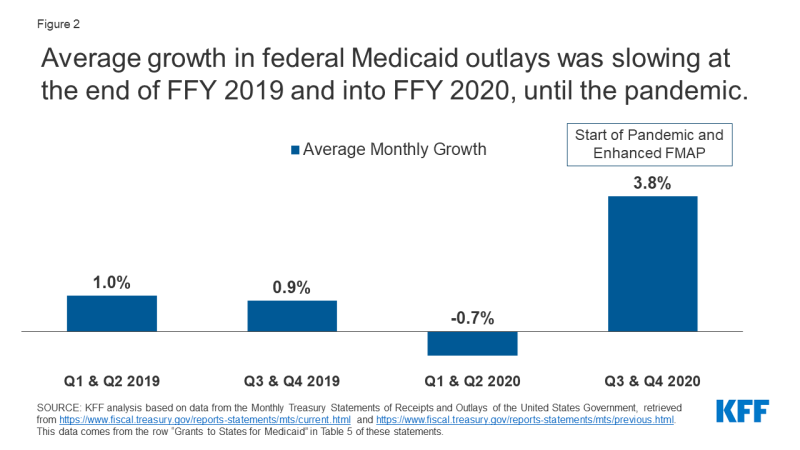
Figure 2: Average federal Medicaid spending growth slowed in late 2019 and through 2020 until the pandemic
There remains uncertainty about the duration and extent of federal tax breaks for government Medicaid programs during the pandemic, which will affect both government and federal Medicaid spending in the future. The FFCRA-approved FMAP increase expires at the end of the quarter that the public health emergency (PHE) ends, which is currently set for January 21, 2021 (which means the extended FMAP is expected to end of the month expires) March 2021). This federal fiscal relief is helping to replace government spending so that growth in federal Medicaid spending can continue to outpace government spending growth as long as the improved FMAP is in place. However, when the tax break expires, federal spending growth will decline and government spending growth will increase sharply. As the recent pre-pandemic temporary FMAP surge (part of the American Recovery and Reinvestment Act of 2009) expired, government Medicaid spending spiked after two years of decline. Similarly, prior to the recent PHE extension, states projected Medicaid spending growth to spike 12.2% in SFY 2021, as most expected the budget relief to end by December 2020 (compared to a projected total spending growth of 8 , 4%). . If the PHE is not renewed again, the phasing out of the FMAP could shift increased Medicaid spending from the federal government to the state governments as enrollment continues to rise and state revenues continue to decline.
In addition to whether the Minister of Health and Human Services will renew the PHE again, it is also uncertain whether Congress can take action to increase the amount and / or duration of the FMAP increase in future COVID-19 pandemic relief bills to increase. The November 2020 presidential election results may also affect future state and federal spending on Medicaid, as President-elect Joe Biden's campaign indicated that his administration would propose the FMAP in response to the Pandemic continues to increase.
Comments are closed.